Preparing for the Night with Insulin-Requiring Diabetes Managing diabetes effectively is a 24/7...
Blog
Why Nighttime Management is the Biggest Unmet Need in Diabetes
Why Nighttime Management is the Biggest Unmet Need in Diabetes
If you live with insulin-dependent diabetes, you know that the day doesn’t end when you go to sleep. For many of us, the night is when the real work begins. It’s a time filled with worry about sudden glucose drops, the blare of CGM alarms, and the exhaustion that follows a night of interrupted sleep. This constant vigilance takes a toll, impacting not just our health but our ability to show up fully for our families, careers, and lives.
For too long, the conversation around advanced diabetes technology has focused on all-or-nothing solutions. But what if the key to better control and more peaceful nights isn't a 24/7 commitment? What if the most significant opportunity for improvement lies in the hours when we feel most vulnerable?
The Best-Kept Secret of Insulin Automation
Automated Insulin Delivery (AID) systems, or pumps, are often presented as the pinnacle of diabetes technology. They promise to reduce the burden of management by automating insulin delivery around the clock. While these systems have helped many, there’s a best-kept secret about where they truly shine: at night.
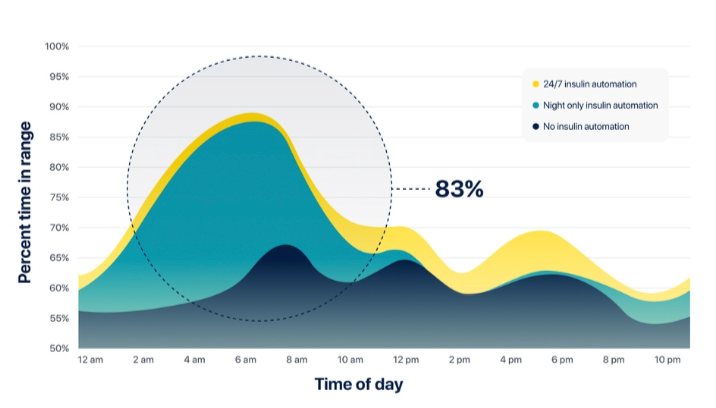
A study comparing 24/7 AID systems with those that automate insulin delivery only at night found a notable difference.¹ The vast majority of the glycemic benefits—over 80% of the improvement in glucose control—actually happen overnight. During the day, when life is unpredictable with meals, stress, and activity, the performance difference between an AID system and an engaged person using a pen is much smaller. But at night, when the body is at rest, automation can predict and prevent fluctuations with incredible precision.
This suggests that the greatest value of automation lies not in its constant 24/7 operation. It’s in its ability to provide a steady hand during the quiet, predictable hours of sleep. This single insight changes everything. It means that you don’t necessarily need a device attached to you all day to get the most important benefits of modern technology.
The Reality for Millions of Pen Users
While the industry often focuses on pumps, most people who use insulin don’t use them. In the United States, approximately 65% of people with Type 1 diabetes and overwhelmingly over 90% of insulin-using people with Type 2 diabetes rely on insulin pens.
Why do so many of us choose pens? For many, it’s a conscious decision rooted in a desire for freedom and bodily autonomy. It’s about not wanting to be physically tethered to a device, managing infusion sites, or dealing with the constant alarms and tubing. It’s about wanting to feel like a person first and a patient second. Yet, this choice for daytime freedom often comes at the cost of nighttime peace. We are left to navigate the darkness alone, relying on alarms and middle-of-the-night corrections that leave us exhausted.
This creates a massive gap in care. An entire community of capable, engaged people is being underserved because the available technology doesn’t fit their lives. They are left facing the most challenging part of diabetes management without the support that could make all the difference.
The Problem with Traditional Pumps
If AID systems work so well at night, why doesn’t everyone just get a pump? The barriers are significant and deeply personal. Beyond the desire for freedom, the practical hurdles make pumps an unrealistic choice for many.
First, there is the cost. Insulin pumps and their disposable supplies represent a substantial financial burden, running tens of thousands of dollars more per year than pen therapy. This high cost can be a significant barrier, even for those with good insurance coverage.
Second is the complexity. Getting started with a pump involves extensive training, and living with one requires managing settings, alarms, and site changes. This complexity can add to the decision fatigue that already weighs so heavily on anyone living with diabetes. Instead of simplifying life, it can feel like adding another full-time job.
Finally, there’s the hassle factor. Wearing a device 24/7 impacts everything from what you wear to how you sleep and exercise. Dealing with irritated infusion sites, kinked cannulas, and the constant physical presence of the device is a burden many are unwilling to accept. For the millions of us who value an untethered life, the compromises of a traditional pump are simply too great.
Luna: A New Way Forward for Nighttime
We believe you shouldn't have to choose between daytime freedom and nighttime peace of mind. That’s why we created Luna. We’ve seen firsthand how technology can improve daytime management, but we’ve always known that the biggest unmet need remained: safe, restful nights.
Luna was born from this understanding. It is designed to bridge the gap, offering the powerful benefits of nighttime automation without the compromises of a full-time pump. Luna works with your existing pen-based therapy, providing automated insulin delivery only when you need it most—while you sleep.
Here’s how it works: you continue to manage your diabetes with your trusted insulin pen during the day, living freely and untethered. At night, you apply the small, discreet Luna patch. It connects with your CGM and uses a sophisticated algorithm to keep your glucose levels stable, protecting you from overnight highs and lows. You get the peace and security of advanced automation without turning your life upside down. You get to wake up feeling refreshed and ready for the day, not recovering from a night of battling your blood sugar.
Reclaiming Your Nights
The future of diabetes care isn’t about forcing everyone onto a single platform. It’s about creating intelligent, flexible solutions that fit into real lives. Nighttime is the frontier where technology can make the most profound impact, offering safety, stability, and the restorative sleep every human being needs.
By focusing on this critical, unmet need, we can finally offer a true third option beyond the false choice of pens versus pumps. It’s time to stop compromising. It’s time to reclaim your nights.
If you’re ready for a solution that provides peace of mind without asking you to sacrifice your freedom, we invite you to join us on this journey.
Footnotes
¹ Kovatchev et al., “Evening and Overnight Closed-Loop Control versus 24/7 Continuous Closed-Loop Control for Type 1 Diabetes.”



